Choosing a note template
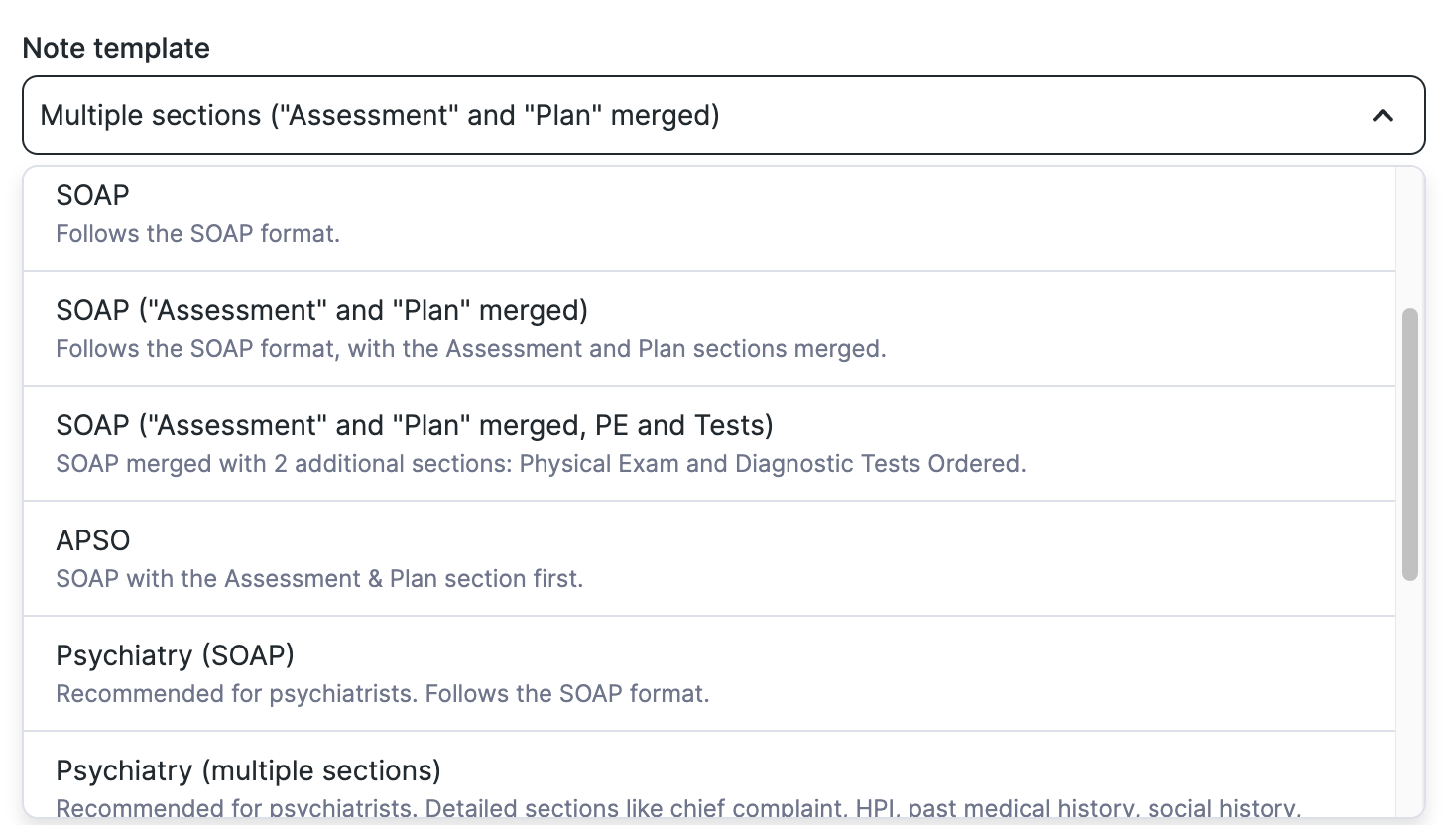
You can select the template of your choice (SOAP, psychiatry, etc.) from the note template dropdown menu.
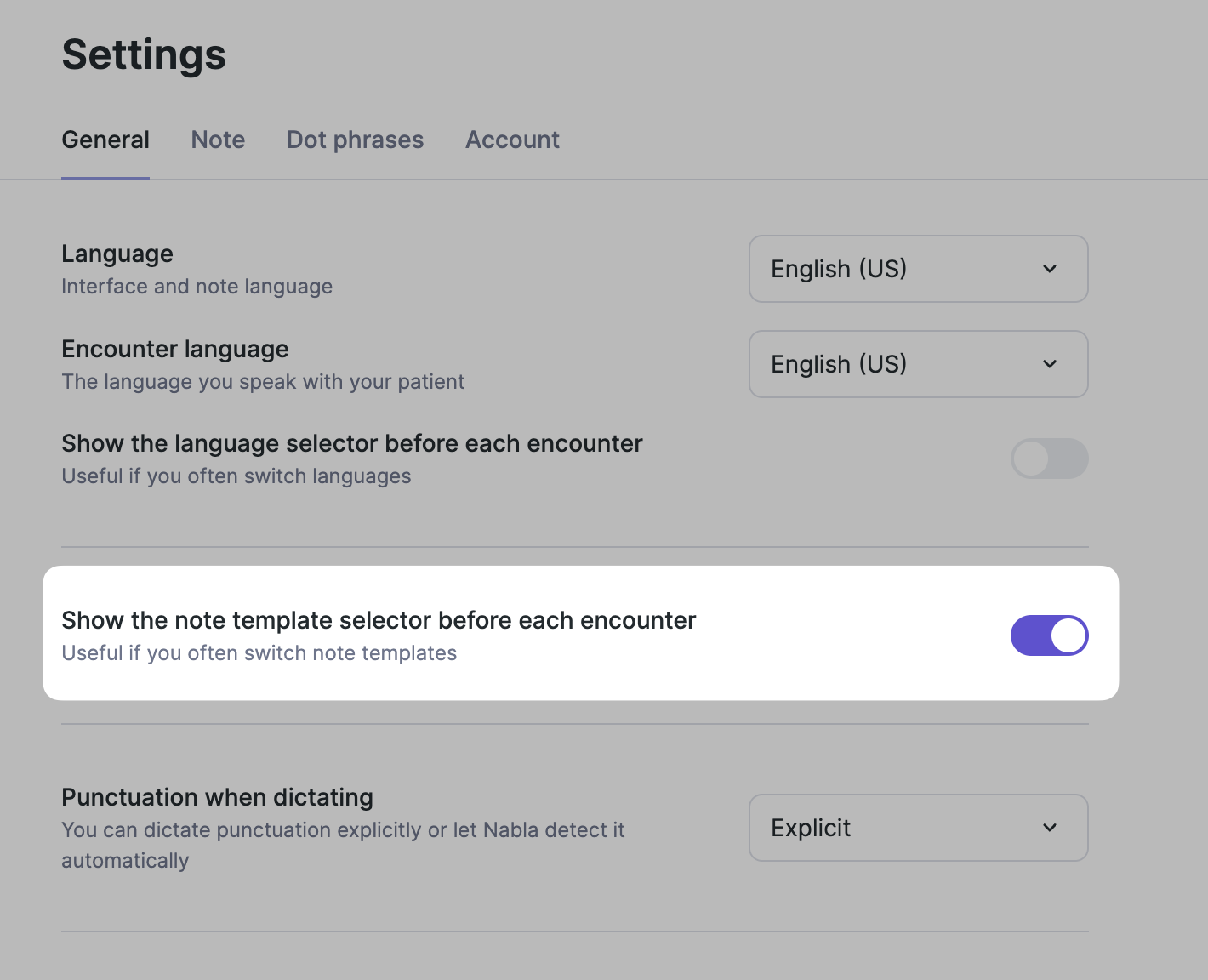
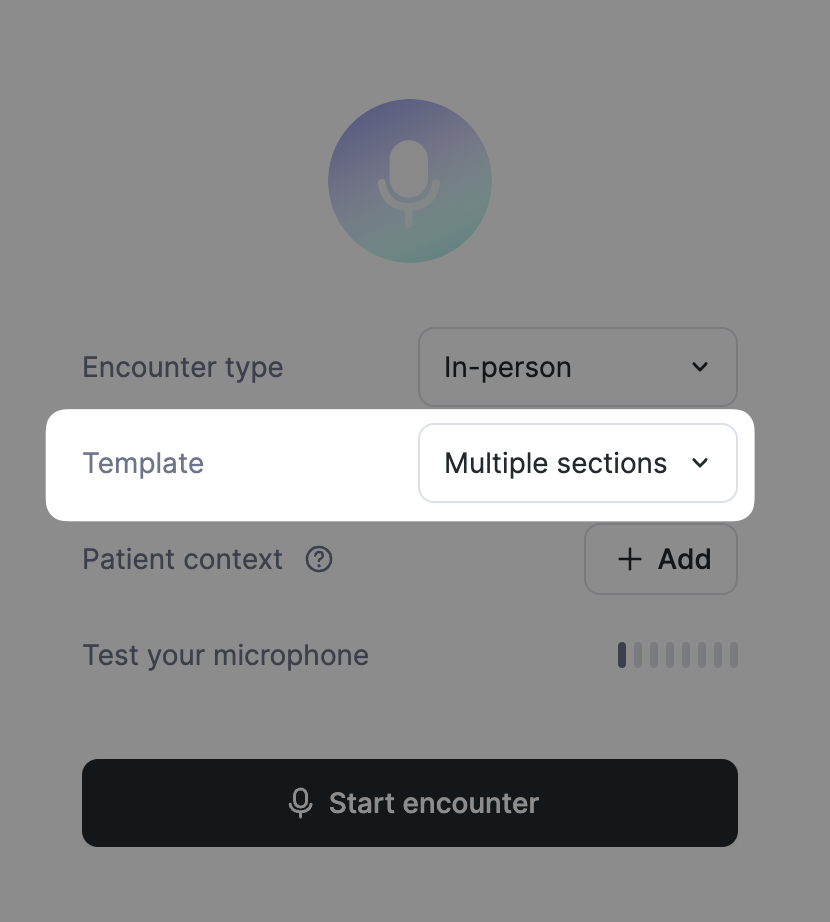
To easily switch between templates before an encounter, enable the template selector on the "New Encounter" screen.
Go to “Settings”
Select the "General" tab
Enable "Show the note template selector before each encounter"
The templates available today :
Template | Sections |
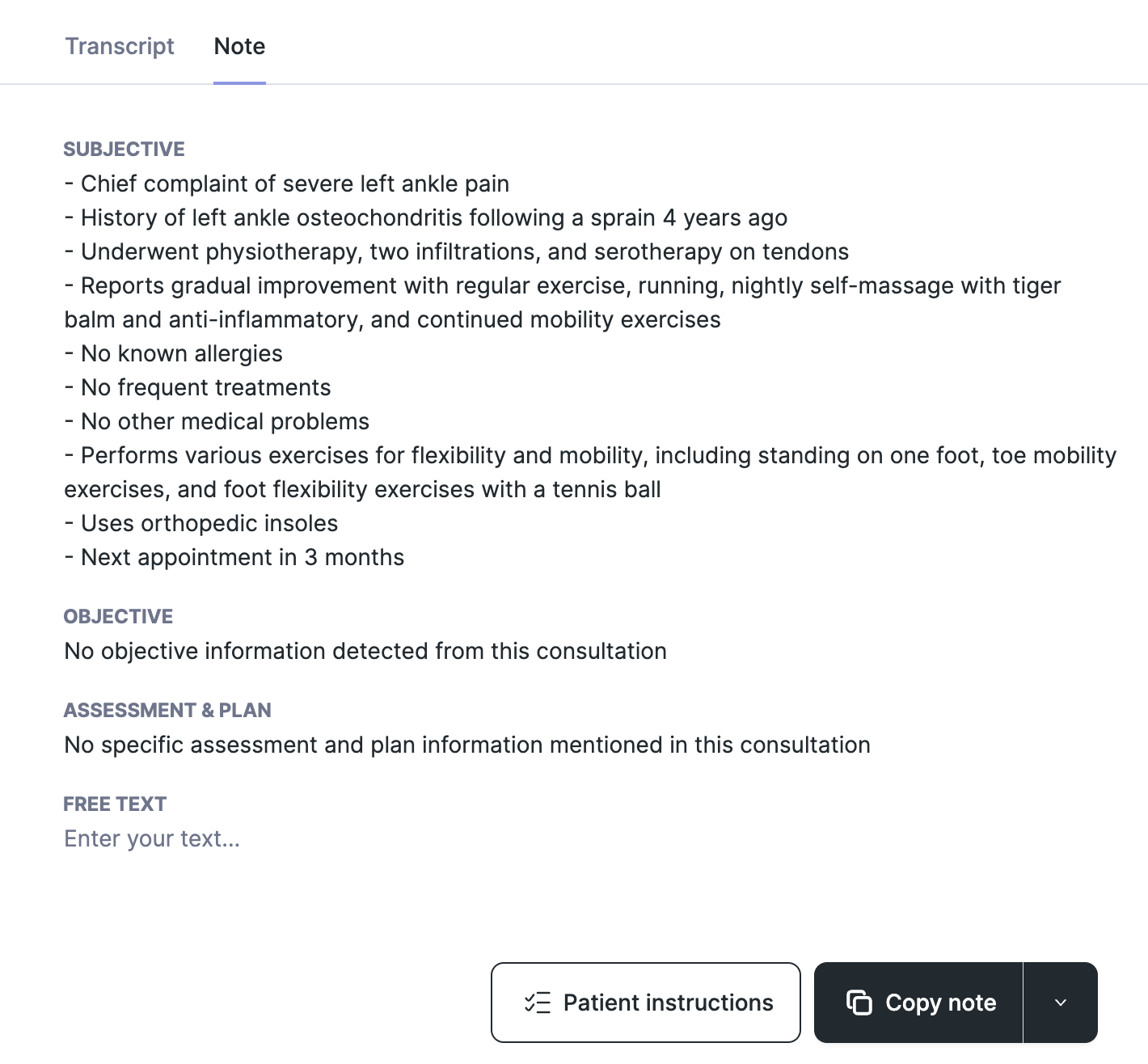
SOAP | Subjective - Objective - Assessment - Plan |
SOAP ("Assessment" & "Plan" merged) | Subjective - Objective - Assessment & Plan |
SOAP ("Assessment" and "Plan" merged, PE and Tests) | Subjective - Objective - Physical Exam - Diagnostic tests ordered - Assessment & Plan |
APSO | Assessment & Plan - Subjective - Objective |
Multiple Sections | Chief complaint - History of present illness - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
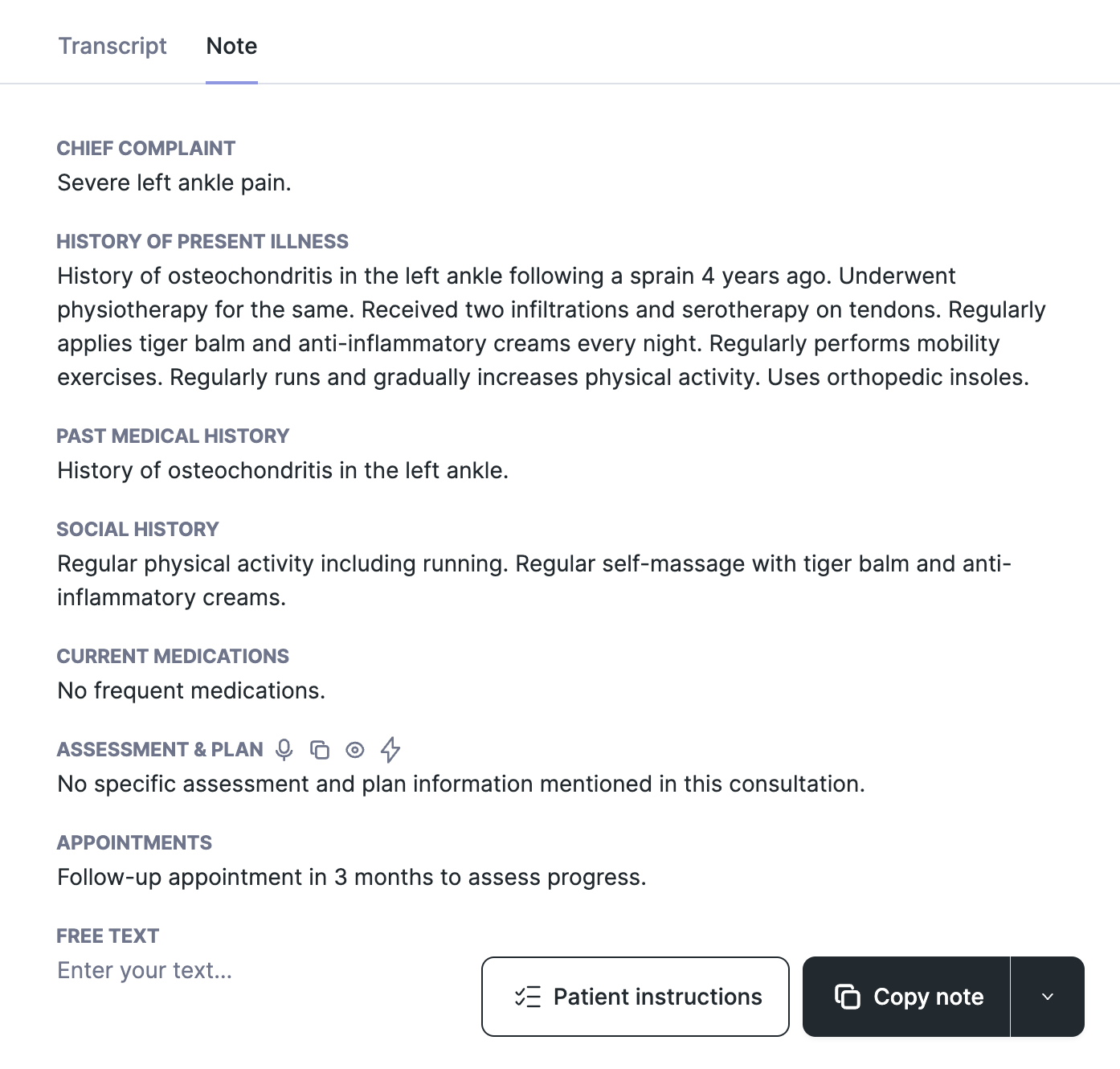
Multiple sections ("Assessment" and "Plan" merged) | Chief complaint - History of present illness - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment & Plan - Prescription - Appointments |
Psychiatry (SOAP) | Subjective - Objective - Assessment - Plan |
Psychiatry (multiple sections) | History of present illness - Chief complaint - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Mental status exam - Plan - Prescription - Appointments |
Cardiology (multiple sections) | Chief complaint - History of present illness - Cardiovascular risk factors - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
Diet (multiple sections) | Lifestyle - Medical history - Reason for visit and goal - Vitals - Food habits - Objective and advice - Appointment |
Psychology (multiple sections) | Chief complaint - History of the present complaint - Mental health history - Social history - Mental status exam - Assessment - Plan - Appointments |
Lactation (multiple sections) | Chief complaint - History of present illness - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
Emergency medicine (multiple Sections) | Chief complaint - History of present illness - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
Emergency medicine (SOAP) | Subjective - Objective - Assessment - Plan |
Well Child Care (multiple sections) | Chief complaint - History of present illness - Well Child Care -Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
Well Child Care (SOAP) | Subjective - Objective - Assessment - Plan |
Oncology (multiple sections) | Chief complaint - History of present illness - Past medical history - Past surgical history - Past obstetric history - Family history - Social history - Allergies - Current medications - Vitals - Immunizations - Physical exam - Lab results - Imaging results - Assessment - Plan - Prescription - Appointments |
Oncology (SOAP) | Subjective - Objective - Assessment - Plan |
Multiple sections (”Assessment” & “Plan” merged) template
SOAP (”Assessment” & “Plan” merged) template